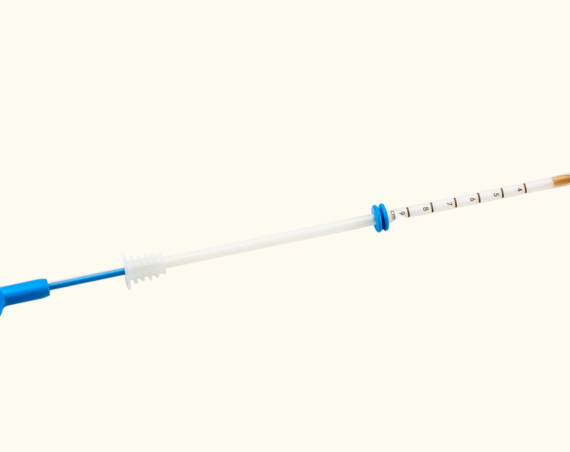
Aetna, a CVS Health company, is now the first major insurer in the US to include intrauterine insemination (IUI) as a covered medical benefit for all eligible plans. This new coverage will be available beginning September 1, 2024, and aims to increase access to fertility services for a broader range of individuals, regardless of sexual orientation or partner status.
Previously, coverage for IUI was often restricted to those who purchased separate infertility benefits or who could demonstrate an infertility diagnosis. Aetna’s policy change simplifies the process, allowing more members to access IUI as both a test of fertility and a means to increase the chances of pregnancy.
“Expanding IUI coverage is yet another demonstration of Aetna’s commitment to women’s health across all communities, including LGBTQ+ and unpartnered people,” stated Cathy Moffitt, MD, Senior Vice President and Aetna Chief Medical Officer, CVS Health. “This industry-leading policy change is a stake in the ground, reflecting Aetna’s support of all who need to use this benefit as a preliminary step in building their family.”
Aetna’s updated coverage is a step towards more equity in health care, particularly in fertility services. The new policy will apply to eligible medical plans nationwide, beginning in September, and will be implemented on a rolling basis for most plans upon renewal. Plan sponsors do not need to make any changes; self-funded plan sponsors retain the ability to modify their benefits, including infertility coverage.
This initiative also supports the company’s broader commitment to transparency in healthcare coverage. Aetna plans to continue making its clinical policies publicly available and regularly updates them to align with the latest clinical guidelines.
Health professionals have welcomed Aetna’s expansion of IUI coverage as a positive step toward reducing financial barriers in accessing fertility care. “We know firsthand the barriers people face in accessing needed medical care to start or grow their families,” said Kate Steinle, Chief Clinical Officer at FOLX, a healthcare provider for the LGBTQ+ community. “We applaud Aetna’s efforts to reduce out-of-pocket costs, so that more people can have the families they dream of – and deserve.”